During Duke University’s 100th year, Duke Neurosurgery marks their 100th patient to receive this innovative procedure
5 Takeaways From This Story
1. HIFU is an incisionless procedure that treats essential tremor and tremor-dominant Parkinson’s disease that does not respond to medication.
2. The results of treatment with HIFU are immediate and can be dramatic
3. During the procedure, the patient is in an MRI machine, and precautions must be taken for patients with pacemakers and other implanted devices. Be sure to discuss this with your doctor when considering this intervention.
4. Essential tremor can run in families; Foster’s uncle had it also.
5. Not all centers offer this procedure. Go here to learn more about the procedure at Duke.

Essential tremor is like a thief, robbing those affected of some of the basic abilities necessary to easily navigate daily life, such as buttoning a shirt or drinking from a cup.
For some, having essential tremor can even feel like a regression. Christopher Foster, 80, of Blairsville, Georgia, described what eating was like with uncontrollable shaking. “It was very problematic,” he said. “I had to drink with two hands and use weighted silverware and a special plate with a rim so I could push the food up against it. I felt like a kid.”
Foster’s wife, Nancy, said her husband used to love fixing things around the house, but the tremors eventually made it hard to hold a screwdriver.
Being able to write with a pen and paper, said Foster, was one of the things he missed most. “Your writing is part of you,” he said, with the emotion evident in his voice. “I used to have such a handsome script.”
On July 17, 2024, everything changed for the Fosters when Christopher became the 100th patient at Duke Neurosurgery to undergo high intensity focused ultrasound (HIFU) for essential tremor.
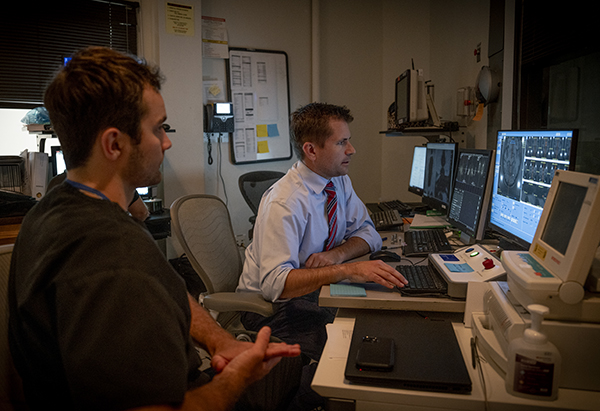
Duke neurosurgeon Stephen Harward, MD, PhD, and team used ultrasound waves to create a pea-sized lesion in the area of the brain responsible for generating the tremors. Within seconds, Foster noticed a dramatic improvement in the tremor.
Duke is one of fewer than 75 hospitals in the country to offer this life-changing treatment.
A Unique Case
Since his tremors began 15 years ago, Foster had tried several medical therapies without success. “You name it, I tried it,” he said. Beyond medication, deep brain stimulation (DBS) is typically the first-line surgical treatment, but for Foster, the invasiveness of DBS was a real concern. He has a pacemaker and takes a daily dose of blood thinner, increasing the risk of a bleeding complication with DBS surgery.
HIFU proved to be an excellent alternative, as the no-incision procedure dramatically lowers the risk of bleeding.
However, HIFU was not without its challenges for Foster, either. During the procedure, the patient is in an MRI scanner. The strong magnetic forces of the MRI potentially interfere with the pacemaker's function. It was for this reason that a medical center closer to the Foster’s home, which also performed HIFU, was reluctant to do so and referred Foster to Duke Neurosurgery.
The Duke HIFU team has had experience safely performing the procedure on patients with pacemakers. Of the first 100 patients, eight had some type of implanted device like a pacemaker. Collaboration between the HIFU team, the MRI team, and the devices’ manufacturers allowed these devices to be put into a safe “MRI mode” during the procedure. Harward and team closely monitor the patient and their heart function with continuous electrocardiogram tracings.
“When we were first starting our HIFU program, we wanted to ensure we could offer this to as many patients as possible,” said Harward. “We specifically chose to perform HIFU on an MRI scanner that allows imaging of these implanted devices. This ability has allowed us to help many who were turned away at other centers.”
Immediate Effects
To prepare for treatment, Foster’s head was shaved, and a metal frame was fitted to his scalp to hold his head during the procedure. He lay on an MRI bed while Harward and team used real-time imaging to target the area in his brain to apply the ultrasound energy.
He did not experience any pain, he said, but was glad when it was over. Immediately afterwards, he experienced dramatic effects, similar to what the 99 patients at Duke before him experienced.
“Unbelievable,” said Foster. “Right away I could take a fork and pick up a single pea from a plate and hold it up in the air perfectly still.”
Return of the “Handsome Script”
Christopher and Nancy's granddaughter is 19 and in the U.S. Coast Guard Academy. During the first seven weeks the “swabs” have no access to their phones or computers, and communication with family and friends must be through the mail. "She said, 'G-Pa, after your HIFU procedure you will be able to write me a letter!'," said Nancy.
Which he did, in his own distinctive handwriting, 24 hours after his surgery.