Translating findings from a lab into patients in a clinic can be a long slog up a steep hill. The new Center for Cancer Immunotherapy helps researchers with the climb.
It’s August 2019, and Duke Professor of Immunology and Pediatrics Tom Tedder, PhD, is excited; a drug initially developed in his research lab is under review by the US Food and Drug Administration for approval to treat a rare autoimmune disease that affects the central nervous system (neuromyelitis optica.)
This excitement was a long time in the making.
The drug, now called inebilizumab, came out of discoveries his lab made more than 15 years ago, about a new way to inhibit immune system cells. Tedder founded a private startup company to develop the drug because, he says, moving it forward using only federal funding “was so slow that I thought I would die before it got to patients.”
Various researchers have estimated that it takes industry an average of 17 years to translate a promising laboratory finding to the clinic. And the average cost to develop a new prescription medication is $2.6 billion, according to a study from the Tufts Center for the Study of Drug Development.
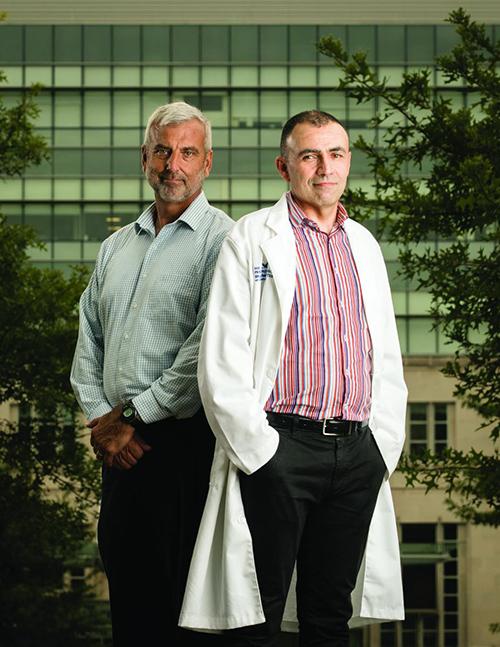
Scott Antonia, MD, PhD, (above, left) aims to speed up this process for scientists across all departments at Duke who have made discoveries that show promise for developing new immunotherapies—treatments that boost the immune system’s ability to kill cancer.
Antonia, who joined Duke in February 2019, is a lung cancer physician who spent years at Moffitt Cancer Center developing immunotherapies to fight lung cancer, including one that in June 2019 changed the standard of care for stage III non-small-cell lung cancer.
Antonia and colleagues who lead the new Duke Cancer Institute (DCI) Center for Cancer Immunotherapy look for cancer immunotherapy discoveries that show promise, no matter the cancer type. Then they form a team that works with the original investigator to accelerate the finding into a drug that can be tested in a clinical trial. The team members will help accomplish all the tasks required to take a finding to human trials, from conducting additional lab studies, to designing a clinical trial, and even manufacturing a drug.
Currently, a dozen or so findings from Duke investigators are under development with the new center. One of those is new work from Tedder’s lab, showing that a particular antibody can selectively decrease a subset of regulatory B cells to ramp up the immune system against cancer. As part of the collaboration, he’s working with physician Neal Ready, MD, PhD, to study the antibody’s activity in cells obtained from human lung cancer patients. “Scott’s new center solidifies everybody’s focus in a common way, and that’s something that is really needed,” Tedder says.
Other findings now in development by the center suggest immunotherapies that will fight head and neck cancer, upper gastrointestinal cancer, colorectal cancer with metastasis to the liver, melanoma, bladder cancer, and lung cancer. Antonia says they will eventually have immunotherapy clinical trials under development for all cancer types.
Mustafa Khasraw, MD, FRCP, FRACP, (above, right) professor in the Department of Neurosurgery and deputy director of the center, is newly arrived at Duke from the University of Sydney (Australia) and brings expertise in designing and leading large clinical trials. “There is enormous hope in the field of cancer research that we can help patients who are now not benefiting from immunotherapy,” he says. Immunotherapies have shown success for some patients with certain cancers, such as melanoma, but not for others. “I think this is the next page in curing cancer. With a lot of us working together, we will get there.”
Antonia says that Duke’s wealth of talent and the willingness of investigators to collaborate is what brought him here. “The science is already here at Duke,” he says. “We just need to accelerate it. We’ve been able to accomplish here in six months what might take years at another institution.”