Report: Brain and Spine Metastasis

Setting a New Standard for Brain and Spine Metastasis Treatment
The Duke Center for Brain and Spine Metastasis (DCBSM), established in 2017, is one of the most comprehensive destination programs of its kind in the country. Highlights of the program include:
- A team-based care approach, with patients meeting with providers from each specialty on the same day –all coordinated by their assigned patient navigator
- Weekly tumor board meetings, where subspecialists pool their knowledge to arrive at the best treatment plan for each patient.
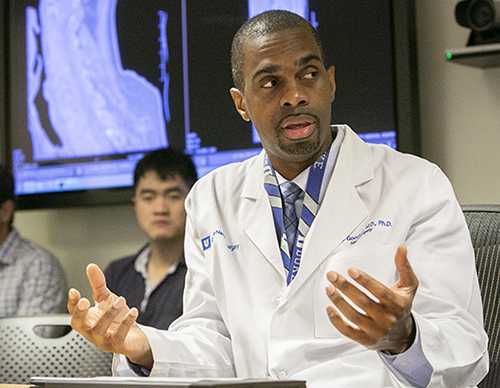
- Access to advanced stereotactic radiosurgery and laser interstitial thermal therapy (LITT). Peter Fecci, MD, PhD, director of the DCBSM, is the country’s highest-volume user of LITT. Rory Goodwin, MD, PhD, will soon begin offering LITT to treat tumors of the spinal column.
Geographic Expansion
The Duke Center for Brain and Spine Metastasis is embarking on an expansion into Wake County, North Carolina, which will enable the center to serve a wider population and provide more accessible streamlined care to patients in the area.
This expansion signifies a substantial commitment to enhancing the treatment and outcomes for individuals with brain and spine metastasis in Wake County and underscores the center's dedication to advancing medical expertise and providing quick and efficient access to state-of-the-art care.

RESEARCH HIGHLIGHT
LITT, Gold Nanostars, and a Veterinary Medicine Collaboration
Laser interstitial thermal therapy (LITT) is a minimally invasive technology that expands therapeutic options for recurrent tumors (GBM and brain metastases), radiation necrosis, and deep-seated lesions that might be difficult to access with craniotomy.
A multi-institutional study led by Peter Fecci, MD, PhD, revealed for the first time that LITT synergizes with post-operative stereotactic radiotherapy (SRT) to produce 4- to 8-fold extensions in freedom from local progression in patients with recurrent brain metastases. Beyond cytoreduction, LITT has also been shown to open the blood-brain barrier and enhance the anti-tumor immune response by causing immunogenic tumor cell death.
While LITT continues to emerge as a standard of care, optimal timing of adjuvant SRT remains unaddressed, and appropriate preclinical models are lacking. Also, non-uniform distribution of heat across tissues limits the size of treatable lesions to 3 cm and can lead to ablation volumes that do not adequately conform to tumor margins.
Addressing these concerns, Fecci and colleagues developed a nanoplatform based on star-shaped gold nanoparticles (gold nanostars) to enhance photothermal ablation. Gold nanostars have plasmonics-active circumferential sharp branches that act as high surface area “lightning rods” that enhance the local electromagnetic field when subject to light stimulation.
They have shown that gold nanostars enhance LITT treatment coverage and specificity in brain phantoms, improve the efficacy and safety of laser ablation in murine tumors in vivo, and selectively collect in murine intracranial tumors when administered systemically. Furthermore, they have shown that gold nanostars amplify the immune benefits of thermal ablation.
Fecci has collaborated with NC State University’s School of Veterinary Medicine to develop the ability to use stereotactic biopsies and LITT in pet dogs suffering from gliomas. They have successfully biopsied and treated four companion canine glioma patients with LITT. Having now proven the feasibility of LITT in dogs, their new goal is to employ these preclinical brain tumor models to further develop the gold nanostar platform for human translation.
All Chapters
Home / Brain / Epilepsy / Cerebrovascular & Skull Base / Pediatric / Chronic Pain / Trauma / Movement Disorders / Brain & Spine Metastasis / Spine / Global / Residency / Top Papers
