Report: Chronic Pain

Neurostimulation Relieves Painful Diabetic Peripheral Neuropathy
Nandan Lad, MD, PhD, offers new hope to patients with diabetic peripheral neuropathy (DPN), with the use of spinal cord stimulation as a neurorestorative treatment.
The results of a 12-month multicenter study published in Diabetes Care demonstrated the sustained effectiveness of 10-kHz spinal cord stimulation from an electrode implanted in the spinal epidural space. Due to the procedure’s relative simplicity, patients can undergo a one-week test procedure before deciding on the permanent implantation of the device, consistingof a minimally invasive procedure consisting of a small electrode and a pacemaker.
Neurostimulation therapy is one component of a multifaceted DPN treatment strategy envisioned by Lad, with clinical management and counseling provided by endocrinologists, podiatrists, neurosurgeons, and neurologists as part of the comprehensive program.
“Remarkably, more than 85% of people had improvement in their neuropathy symptoms and 66% experienced some neurological improvement including many regaining sensation in their feet for the first time in years,” said Lad. “This represents the first truly neurorestorative treatment for DPN.”
DREZ Relieves Spinal Avulsion Pain When Other Options Fail
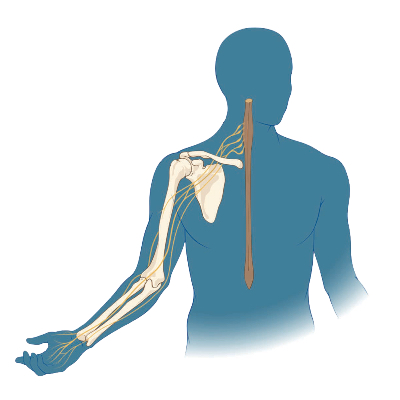
Duke pioneered the dorsal root entry zone (DREZ) procedure to relieve the phantom pain from an injury when other pain treatment options have failed.
The technique originated at Duke—it was often called Nashold’s procedure in the early literature, because former Duke neurosurgeon Blaine S. Nashold, MD, first described it in the 1970s. Duke’s Allan Friedman, MD, assisted in the
development of the procedure, developing new instruments to minimize complications and wrote a number of early articles about DREZ.
“A majority of the cases we treat are patients with upper extremity, high-velocity injuries from accidents in cars, boats, and the like, in which the brachial plexus is stretched or torn,” said Nandan Lad, MD, PhD, who specializes in chronic pain. “When the nerve is separated from the spinal cord, the spinal cord interprets that missing input as pain. When medications and interventional treatments aren’t helping, the DREZ procedure can silence those missing inputs.”
The surgery involves identifying the areas of injury and ablating the injured nerves. It is a delicate surgery that requires an experienced team to map the spinal cord.
“We have an excellent intraoperative neuromonitoring team led by neurologist Aatif M. Husain, MD, that helps map the area where the injury has occurred,” Lad says. “I am very conservative in terms of making a lesion because it can be permanent. We do a test stimulation and map the response on the neuromonitoring while the patient is under anesthesia. We test motor function before and after every lesion using motor evoked potentials. We ablate the missing inputs from top to bottom of the avulsed nerve root region. It is a team effort to make sure it is done as safely as possible.”
When the injury involves the lower cervical spine, Lad enlists the help of a Duke neurosurgical spine specialist Muhammad Abd-El-Barr, MD, PhD.
All Chapters
Home / Brain / Epilepsy / Cerebrovascular & Skull Base / Pediatric / Chronic Pain / Trauma / Movement Disorders / Brain & Spine Metastasis / Spine / Global / Residency / Top Papers
