Report: Cerebrovascular and Skull Base

Wire sculpture by Samatha Spellicy, MD, PhD (PGY2)
RECENT ACCOLADES
-
Duke’s skull base surgery team has been named a Multidisciplinary Team of Distinction by the North American Skull Base Society (NASBS). This designation recognizes a multidisciplinary approach to patient care by a comprehensive team of sub-specialists.
-
Duke has been named a Center of Excellence for the treatment of cerebral cavernous malformations (CCM) in both adults and children. The designation by the Alliance to Cure Cavernous Malformation recognizes the hospital for providing expert, integrated, multi-disciplinary care and cutting-edge research to CCM patients and their families. It is the only CCM Center of Excellence in North Carolina.
-
In June 2023, Duke hosted the International Conference on Subarachnoid Hemorrhage, attended by specialists from around the world.
Vein of Galen Malformation: Procedure Today, Home Tomorrow
Erik Hauck, MD, treats vein of Galen malformation with endovascular embolization, a minimally invasive procedure that allows patients to go home as soon as the next day. In the recent case involving a six-month-old baby, the child was diagnosed in utero, and Hauck and a team of specialists was waiting to assess him at birth. The team determined immediate treatment was not necessary, but six months later an MRI showed that the malformation had grown, and surgery was scheduled.
Hauck inserted a microcatheter into the right femoral artery and guided it to the malformation. He used a medical-grade glue to shrink the opening, choking off the malformation’s blood supply and redirected blood back to the organs. The procedure required no incision, but only a small needle stick.
Awake Surgery for Enovascular Brain Aneurysm Repair Lowers Risks, Speeds Recovery

Neurosurgeon David Hasan, MD, performs awake surgery for unruptured brain aneurysm for patients who want to avoid general anesthesia. Hasan uses an endovascular approach to place a flow- diverting stent. A catheter is threaded through a major artery in the groin and up to the aneurysm. Then a stent is placed to direct blood flow away from the area. Patients remain conscious but sedated
during the procedure and communicate with the surgeon, which helps in monitoring critical brain functions. Awake surgery also makes endovascular surgery available for people with life-threatening aneurysms who cannot undergo general anesthesia, including those with diseases like chronic obstructive pulmonary disease (COPD) and pulmonary hypertension.
Team-Based Care for Moyamoya Disease
Duke is a national referral center for moyamoya disease and one of a few academic medical centers in the world with multiple specialists who have experience caring for children and adults with the condition. When Gerald Grant, MD, returned to Duke from Stanford, he added his moyamoya expertise in pediatric and young adult cases to that of Ali Zomorodi, MD, who specializes in adult cases.
As a referral center in the Southeast, Duke consults on complex cases, confirms diagnoses, and cares for patients who have been turned away elsewhere.
“It’s not enough for a patient to get great care by one individual,” said Grant. “They must trust that they are getting the best possible care by a team.”
Patients receive a full workup and advanced imaging studies, which may include magnetic resonance angiography, computed tomography angiography, or cerebral angiography. The surgeon then reviews the case with experts in related disciplines to determine the best course of action for revascularizing the brain.
Treatment requires a complex and time-sensitive direct or indirect cerebral artery bypass to reroute blood flow around the stenotic or occluded artery. “You’re on the clock because you need to perfuse the brain as soon as possible again after clamping the blood vessels and interrupting the blood supply,” he said. “Because of this, the stroke risk for this procedure is temporarily higher because you need to isolate the donor vessel, usually in front of the ear, and hook it up to one of the brain blood vessels to bypass the blood flow.”
Many Disciplines, One Plan: The Multidisciplinary Pituitary Clinic
In a new approach to pituitary disorders, the departments of Neurosurgery, Head and Neck Surgery, Endocrinology, and Ophthalmology team up to offer patients a one-stop, multidisciplinary clinic.
“When a referral comes in, I’ll review and triage referral to determine which provider or combination of providers the patient should see,” said Denise Lally-Goss, ANP-C, GNP-C. “The patient will be scheduled for our dedicated pituitary clinic.”
These benefits make for high satisfaction among patients as well as providers, according to Lally-Goss. “Patients love seeing multiple providers in one location, back-to-back, which minimizes wait time.”
The benefits of the multi-disciplinary clinic include:
- Convenience for Patients: One trip for multiple appointments, less time off work, less travel expense
- Multidisciplinary Planning in Real Time: Instead of waiting for call backs, patients leave with a plan
Novel Neurophysiologic Monitoring Techniques in Vestibular Schwannoma Surgery

One of the major causes of morbidity following surgery for vestibular schwannoma is damage to the nerve that controls facial expression.
“Damage to the facial nerve can result in decreased quality of life, and preservation of the nerve is one of the major
considerations that limits the extent of surgery,” said Ali Zomorodi, MD, cerebrovascular and skull base neurosurgeon. “This is can increase recurrence risk and the increase the potential need for re-operation.”
Monitoring the facial nerve intraoperatively typically involves stopping surgery to stimulate the nerve to ensure functioning, but Zomorodi and team have developed a better solution.
“The solution we’ve come up with allows the surgeon to receive feedback about the integrity of the facial nerve without having to pick up the stimulator,” he said. Working with Duke electrophysiologists, Zomorodi and team are using a continuous feedback system that triggers the blink reflex by stimulating an electrode on scalp. The system doesn’t require any stopping the surgery or any extra steps by the surgeon.
The team has been using the feedback system with all vestibular schwannoma for the past 18 months.
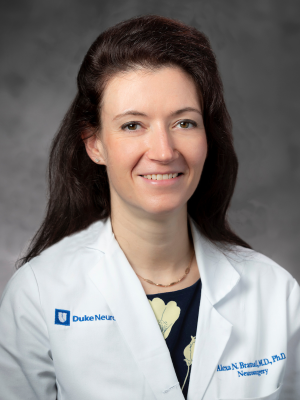
Coordinated Care for Patients with Normal Pressure Hydrocephalus
Normal pressure hydrocephalus (NPH) may affect up to 5% of individuals over 80 years of age. The condition is often mistaken for other neurological disorders like Alzheimer's and may lead to multiple falls, significant cognitive changes, and urinary problems.
Duke Neurosurgery is developing a coordinated effort to create a unified protocol for diagnosing and treating patients with NPH. This multidisciplinary team includes neurology, neurosurgery, and physical therapy.
The team also plans to conduct research focused on molecular profiling of samples
from cerebrospinal fluid and enabling patient access to cutting edge neuroimaging techniques. “These methods have the potential to yield greater insights into the pathophysiology of NPH and, in combination, may better identify patients who may benefit from neurosurgical intervention,” said neurosurgeon Alexa Bramall, MD, PhD.
The ultimate goal is to provide superior care for NPH patients with evidence-based strategies and new technologies to help diagnose and successfully treat patients.
RESEARCH HIGHLIGHTS
MACHINE LEARNING TO AID IN CLASSIFYING SKULL BASE TUMORS DURING SURGERY
In the lab of neurosurgeon Patrick Codd, MD, researchers have developed a fluorescent detection method that uses machine learning to aid in classifying tumors during surgery to guide precise tumor removal. Codd’s team has successfully used this technology in pituitary tumor surgeries, and it may improve outcomes in other skull base tumors. They presented their results at the North American Skull Base Society annual meeting in February 2023.
MOLECULAR TARGETS FOR SKULL BASE MENINGIOMAS AND VESTIBULAR SCHWANNOMAS
Duke clinician scientists are working to identify molecular targets that are signature unique to both meningiomas and vestibular schwannoma. “Successful identification would enable the design of pharmaceutical agents or immunotherapeutic molecules that could target these two tumors and be used as a primary or adjunct treatment,” said David Hasan, MD.
Concurrently, the team is working on designing nanoparticles that could be used as a “Trojan horse” carrier for chemo-agents or other therapeutics, These iron oxide nanoparticles could also be used as MRI imaging tracers to monitor successful targeting of these tumors.
EMERGING IMAGING TOOLS TO BETTER PREDICT ANEURYSM RISK
Historically, determining whether to observe an unruptured brain aneurysm or operate has mostly hinged on the aneurysm’s size and location. But that paints an incomplete picture, says David Hasan, MD, who has been working for decades to improve brain aneurysm diagnosis and treatment. He and his colleagues at Duke are using sophisticated imaging tools to help determine the best next steps:
Molecular Imaging with Ferumoxytol
Ferumoxytol is an injectable medication used to treat people with chronic anemia. Before coming to Duke, Dr. Hasan and his team discovered that the ferumoxytol molecule acts like a contrast agent when used with MRI imaging to detect specific inflammatory cells responsible for aneurysm eruption.
High-Resolution Vessel Wall Imaging
This technique uses traditional MRI contrast called gadolinium. By suppressing a specific MRI signal, the contrast pools in the area between the inner wall of the brain aneurysm and the blood inside. A white color indicates that the aneurysm has active changes, increasing the risk of rupture.
Quantitative Susceptibility Mapping (QSM)
QSM is a specific setting or sequence that is added to an MRI scan to help detect and measure micro-bleeds – when trace amounts of blood leak through thin areas of the aneurysm wall – that can signal a rupture is coming.
Computational Dynamics
This method uses MRI and computer modeling to measure how fast blood moves through the aneurysm, with slower movement being associated with aneurysm deterioration.
Finite Element Analysis
Finite element analysis uses MRI technology to assess the strength and elasticity of the brain aneurysm wall.
